TL;DR
Employers must ensure pregnant workers’ safety post-exposure (e.g., whooping cough) under OSHA and PWFA. Provide preventive care, testing, or accommodations, and consider family care costs to avoid legal risks. Coordinate with the employee’s doctor, document decisions, and update safety policies to protect expecting staff and their families.
Hey there, HR pros—if you’re reading this on Decision Makers Hub, you know how tricky it gets when workplace safety bumps up against family life. Picture this: a team member in healthcare or a high-contact role tells you they’ve been around a contagious bug like whooping cough while expecting a baby. It’s not just about following rules; it’s about keeping your people safe and supported. This guide breaks it down into straightforward questions, like a chat over coffee, so you can step in confidently. We’ll stick to the basics on what laws say, what experts recommend, and how to handle those tough spots where work health advice clashes with a doctor’s take.
What Counts as a Workplace Exposure Risk for Expecting Employees?
Think of exposures like whooping cough (also called pertussis) as sneaky threats in jobs where folks care for patients or kids. These bugs spread through coughs and close contact, hitting harder on little ones and moms-to-be. For your company, the big question is: does the job put someone at higher odds of catching it? Federal rules from groups like OSHA say yes if it’s part of daily duties, like nursing or teaching.
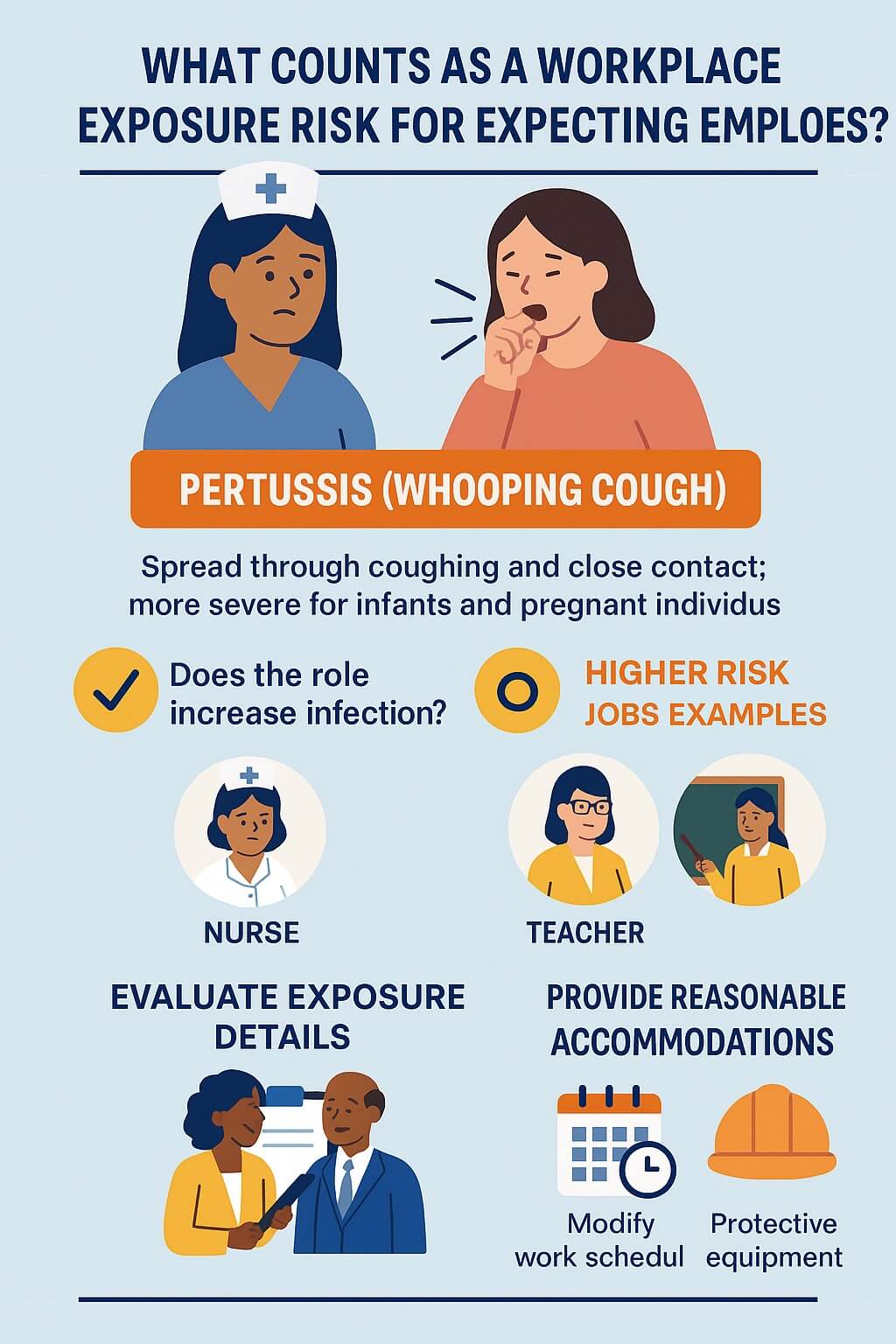
Your first move? Chat right away with the employee and their boss to map out the details—when it happened, how close the contact was, and any symptoms popping up. Don’t guess; pull in your occupational health team or a safety expert to size up the real danger. Laws like the Pregnant Workers Fairness Act (PWFA) kick in here, pushing you to tweak schedules or spots to cut risks without sidelining anyone. It’s about smart fixes, like shifting to desk work or extra gear, so everyone stays healthy and on the payroll.
Do Employers Have to Offer Preventive Meds or Shots to Pregnant Staff After an Exposure?
Short answer: often yes, but it’s not one-size-fits-all. Health guides from the Centers for Disease Control and Prevention (CDC) suggest preventive antibiotics for close contacts of someone with whooping cough, especially if they’re pregnant or around newborns. The catch? These meds come with pregnancy warnings—use them only if the upside beats the downside, like protecting a baby from severe illness.
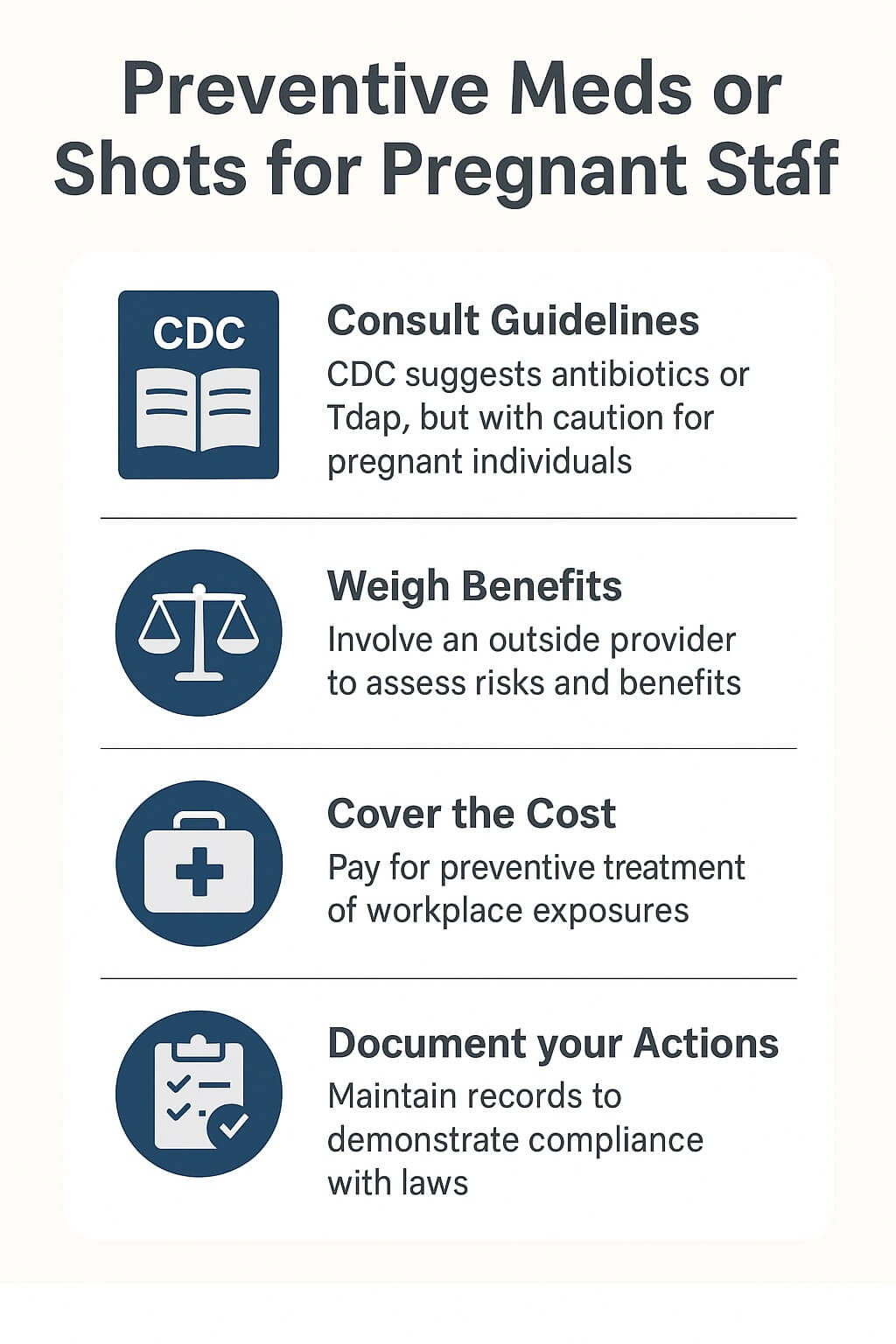
As HR, you’re on the hook to make sure your health pros weigh this carefully, looping in the employee’s own doctor early. If shots like Tdap (a booster for whooping cough) are due, the CDC pushes for one in the third trimester of every pregnancy to pass protection to the baby. Your role? Cover the cost if it’s tied to the job exposure, and document everything to show you’re acting in good faith. Skipping this could open doors to claims under PWFA or even the Americans with Disabilities Act (ADA) if the pregnancy ties to a short-term health limit.
Why Won’t Work Health Always Test for Bugs Like Whooping Cough Right Away?
Testing sounds simple—swab and know—but it’s not always the go-to. CDC folks say for mild coughs after exposure, they lean toward preventive steps over tests, since early signs can mimic a cold from daycare or elsewhere. Tests work best when symptoms ramp up, like that classic whooping sound, but waiting might mean the bug’s already spreading.
If your employee pushes for a test (smart, to protect family), listen up. Under OSHA’s general safety duty, you can’t just say no without a solid reason. HR tip: bridge the gap by offering paid time for their personal OB to order it, or tap an outside lab if your in-house setup drags feet. This keeps trust high and avoids gripes about unequal treatment. Remember, pregnancy amps up worries about passing illness home, so err on the side of caution—it’s cheaper than a lawsuit.
What Happens When Occupational Health Advice Clashes with an OB’s Recommendations?
This is the sticky part: your work clinic says hold off on meds due to pregnancy risks, but the OB wants action now. Who’s right? Neither “side” is always wrong—it’s about the full picture. Federal protections like PWFA require you to chat with the employee, review both views, and land on a plan that fits her needs without undue hassle for the business.
Step one for you: set up a quick huddle with all parties (with her okay on sharing info). If the OB calls for testing or a different treatment, don’t block it—offer flexibility like adjusted shifts to make the appointment. On costs: if your plan covers it as work-related (think workers’ comp for exposures), foot the bill. But if benefits run through another job? That’s trickier—check your policy, and consider bridging with short-term aid to show support. Courts love when employers play fair, so keep notes on why you chose one path.
Are Companies Liable for Extra Costs if a Pregnant Worker’s Family Needs Care Too?
Family ripples are real—if mom gets exposed, hubs and kids might too. Your duty stops at the employee, but smart HR stretches further. OSHA pushes safe workplaces to prevent spreads, so if inaction leads to home illnesses tied to the job, you could face claims. For instance, if no test means no alert for household prophylaxis, that’s a red flag.
Advice: build a chain-of-care plan. Offer resources like free family shots if guidelines back it, or point to low-cost clinics. Under ADA, if pregnancy limits count as a disability, accommodations might include family leave buffers. Bottom line: covering extras like a family doc visit can prevent bigger headaches, and it builds loyalty. If budgets pinch, start small—maybe partner with local health orgs for free events.
How Can HR Spot and Fix Gaps in Pregnancy Safety Policies?
No one’s perfect, but you can level up. Start with a fresh look at your safety playbook: does it flag high-risk roles for expecting folks? Add pregnancy chats at hire and check-ins, per NIOSH tips for work hazards. Train managers to spot signs—like fatigue from exposures—and route them to you fast.

For conflicts, bake in a neutral review step, maybe with an outside expert. Track trends too; if multiple reports pop, it’s time for broader fixes like better ventilation or rotation schedules. PWFA deadlines mean acting quick—accommodations can’t wait. End goal? A workplace where expecting team members feel backed, not burdened.
Where Do HR Leaders Turn for Backup on These Issues?
You’re not solo. Hit up OSHA’s free consults for tailored safety audits, or CDC’s pregnancy work guides for exposure how-tos. For legal angles, EEOC’s site spells out PWFA and ADA must-dos. Local groups like state labor boards offer webinars, and tools like employee handbooks can weave this in yearly.
One last nudge: talk to your legal eagle early on exposures—better safe than sorry. Got a story or snag? Drop it in the comments; we’re all in this to make work kinder for growing families. Stay steady out there.
